It’s a question… not a statement.
When analyzing Alzheimer’s Disease (AD) from a multi-pronged perspective, it’s clear that there are numerous factors involved in the pathology of this illness. AD is formally considered to be an irreversible, progressive brain disorder that impairs memory and thinking skills coinciding with brain atrophy. There have been decades of research and billions of dollars that have gone into developing pharmacological approaches to addressing AD with very little success thus far. How could it be possible that a relatively simple breathing technique could effectively assist in combating this disease?
While much of the predominant discussion surrounding AD has been in regards to an accumulation of beta-amyloid protein, there appear to be other consistent abnormalities associated with the illness.
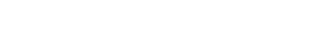
Decreased Cerebral Blood Flow
One of the consistent abnormalities observed throughout AD progression, pre-clinical phases of AD and even cognitively healthy subjects at high-risk to develop AD is hypoperfusion (reduced cerebral blood flow). Sufficient cerebral blood flow (CBF) is key for the proper delivery of oxygen and metabolic nutrients to the brain. A 2011 review in the Journal of Alzheimer’s Disease outlined numerous studies utilizing various forms of measurement (SPECT, MRI, PET) to quantify and verify this occurrence of hypoperfusion in AD. Reductions in CBF have been observed from 10 to 28% in subjects with AD. A 2018 study published in the American Journal of Translational Research observed that hypoxia (low oxygen levels) promotes the accumulation of beta-amyloid protein in the brain via inducing increased interaction between the CD147 and Hook1 genes.
Cerebrospinal Fluid Aberrations
Cerebrospinal fluid (CSF) is a clear, colorless fluid that surrounds the brain, is found within the brain tissue as well as throughout the spinal cord. CSF is also responsible for removing waste products from the brain as well as maintaining the proper function of the central nervous system. A 2001 study published in the journal Neurology observed that patients with Alzheimer’s disease had a marked reduction in CSF production. The researchers observed that Alzheimer’s patients produced 50% less CSF than average secretory rates. A 2017 study published in the Journal of Nuclear Medicine found that patients with AD had markedly decreased CSF clearance compared to control subjects. The researchers found a 23% decrease in CSF clearance and a 66% fewer superior nasal turbinate CSF drainage sites. A 2019 study published in the journal Frontiers in Aging Neuroscience observed that decreased cerebrospinal fluid (CSF) flow is associated with cognitive impairment in the elderly. The researchers found that patients with lower CSF flow had significantly worse memory, visuoconstructive capacities, and verbal fluency.

Compromised Lung Function
While the relationship between lung function and brain health might not be obvious at first glance, based on the direct influence of cerebrospinal fluid movement by respiration as well as the effects of breathing on cerebral blood flow, there appears to be an important underlying connection. A 2015 review in the journal Alzheimer’s Research & Therapy presents a multitude of data points indicating that there is a strong association between cognitive impairment and impaired lung function. A 2019 study in the American Journal of Respiratory and Critical Care Medicine analyzed a total of 14,184 subjects over multiple decades and also found a correlation between impaired lung function and an increased risk of dementia later in life.
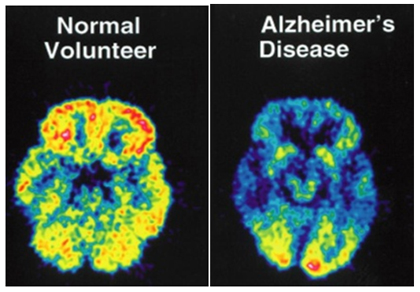
Brain pH Decreases (Acidification)
A 2006 study published in the journal of the Proceedings of the National Academy of Sciences observed that hypoxia (reduced oxygen and decreased pH) facilitates AD pathogenesis by upregulating BACE1 gene expression. This coincides with decreased cerebral blood flow also observed in AD. A 2018 study published in the journal Frontiers in Neuroscience observed that exposing animals to acute hypoxia could induce AD-like pathological damage. Animals exposed to one single episode of hypoxia over 24 hours had increased expressions of amyloid precursor protein (APP), anterior pharynx-defective 1 (APH1) and cyclin-dependent kinase 5 (CDK5). In addition, these animals exuded neuroinflammation and abnormal mitochondrial function. A 2021 meta-analysis published in the journal Neurobiology of Aging found that AD is associated with decreased brain pH and decreased CSF pH in humans. It was also cited that low extracellular pH increased amyloid-beta plaque load in animal models of AD.
Neurogenesis disruption
Neurogenesis is the process by which new neurons are formed in the brain. A 2019 study published in Nature Medicine observed that adult hippocampal neurogenesis is abundant in healthy subjects while dropping sharply in patients with Alzheimer’s disease. A 2021 study published in Cell Reports identified the genetic mutations correlated with altered neurogenesis in AD patients. The researchers identified presenelin-1 (PSEN1) as the gene responsible for neurogenesis disruption.
Gamma Oscillation Abnormalities
Gamma oscillations are brain waves that are considered to be the fastest measurable oscillations starting at 35 Hz and going up to 200 Hz (or more). A 2006 study in The Journal of Neuroscience observed that theta-gamma oscillation synchronization predicted encoding and retrieval of memories. A 2018 study in the journal Frontiers in Aging Neuroscience observed that AD patients exuded the lowest level of theta-gamma synchronization compared to mild cognitive impairment and healthy subjects. A 2020 study published in Neuroimage observed that gamma oscillation weakening is a natural part of aging. This general weakening of gamma oscillations in the elderly potentially coincides with less robust memory retrieval in the elderly with or without AD.

Wim Hof Method (WHM)
Now that we’ve identified the various periphery physiological correlations associated with AD, let us take a look at the WHM breathing exercise (not cold exposure due to potential AD patient intolerance) and the potentiality for it to address these conditions. Generally speaking, the WHM breathing technique consists of roughly 30 deep inhalations with passive exhalations. The final exhalation is a forceful complete emptying of the lungs immediately followed by a breath hold of 30 seconds or more. Following the breath retention, a deep inhalation takes place which is then held for 10 seconds. This entire process constitutes one “round” of WHM and is generally repeated for a minimum of 3 rounds for optimized effect.
It seems evident that cerebrospinal fluid (CSF) movement in the brain is predominantly driven by respiration. A 2015 study published in The Journal of Neuroscience outlined the discovery that during forced breathing, high CSF flow was elicited during inspiration (breathing in). Being that WHM focuses on deep inhalations followed by passive exhalations, it seems clear that inducing increased CSF movement and CSF volume in the brain is definitively taking place during the process. It is believed that lymphatic drainage of the brain occurs based on a decrease in thoracic pressure driven by inspiration. A 2005 study in the journal Experimental Biology and Medicine observed that the choroid plexus (the predominant site of CSF production) also plays a key role in removing amyloid-beta from the CSF. While the initial deep breathing cycle of WHM increases CSF movement, it also causes vasoconstriction (narrowing of blood vessels) leading to a temporary decrease in cerebral blood flow (CBF). However, the reduction in CBF is short-lived being that the deep breathing is followed by breath holding which leads to an increase in CBF greater than levels seen at baseline. A 1999 study published in the American Journal of Neuroradiology observed that breath retentions lasting 40 seconds increased CBF in certain regions of the brain by up to 87%. A 2015 study in the Journal of Cerebral Blood Flow & Metabolism observed the effects of prolonged breath retention in elite divers and noted a 100% increase in CBF compared to baseline. This is likely taking place due to the increase in carbon dioxide (CO2) from the breath holds which leads to dilation of the arteries and capillaries of the brain.
There lies the potentiality that WHM breathing technique mimics some of the cerebral effects of cardio exercise due to the respiratory fluctuations and alterations in both CSF movement and CBF. A 2010 study published in the Journal of Neuroscience found that 30 minutes of moderate intensity exercise increased CBF by 20% up t0 30 minutes following the cessation of the activity. A 2020 study published in the journal Cerebral Cortex observed that 20 minutes of moderate intensity exercise increased CBF by 10 to 12% in the hippocampus area of the brain for up to 60 minutes following the end of exercising. A 2020 study published in the Journal of Cerebral Blood Flow and Metabolism observed that increasing CBF in animals with late stage AD improved cognition.
One of the by-products of WHM in regards to producing increased CSF movement as well as inducing increases in CBF following the practice is the obvious effect on blood pH. In a 2014 study published in the journal Proceedings of the National Academy of Sciences it was observed that WHM breathing caused an increase in blood pH of up to 7.76 in some subjects (baseline is 7.2 to 7.4). A 1994 study in the journal Neurosurgery found that CSF pH rapidly follows arterial blood pH with changes in respiration. This seems increasingly important in light of the data indicating that Alzheimer’s patients have been observed to have decreased brain and CSF pH compared to controls (as cited above). According to the latest data, apolipoprotein E4 (APOE4) is the leading genetic risk factor associated for AD and is directly associated with impaired amyloid beta clearance. A 2018 study in the journal Proceedings of the National Academy of Sciences observed that amyloid beta clearance defect in astrocytes (brain glial cells) expressing APOE4 is caused by excessive acidification of the epigenetic microenvironment which could be reversed by alkalinizing the endosomal pH environment. The researchers of the study proposed the possibility that repurposing drugs that alkalize endosomal pH could be a potential viable pathway to addressing neurodevelopment and neurodegenerative disorders. According to the Alzheimer’s Association 4 genes have been closely correlated with AD risk… APOE4, Presenelin-1 (PS-1), Presenelin-2 (PS-2), and amyloid precursor protein (APP). It also appears that all 4 of these genes are directly affected by microenvironmental fluctuations in pH. A 2015 study in the Journal of Molecular Biology observed that APP activity is distinctly modulated by pH levels. A 2015 study in the journal Cell Reports indicates that PS-1 modulates calcium signaling via responses to pH changes. A 2020 review in the journal Cells outlined similar pH influence on calcium signaling modulation by PS-2.
Since WHM induces increases in pH, it would seem plausible that an entire cascade effect of genes related to AD experience a downregulation from the breathing technique. The main question is for how long the downregulation would be sustained and how often the WHM technique must be practiced in order to retain it’s effect.
This brings us to the compromised lung function aspect of AD. Since it appears fairly straight forward that WHM drives CSF movement, modulates CBF, and increases brain/CSF pH based on breathing… it should come as no surprise that shallow breathing would in essence create the opposite… poor CSF movement, impaired CBF, and decreased pH. The question is whether compromised lung function is progressively permanent or whether WHM can improve and/or reverse the condition. A 2011 study in the journal Clinics observed that lung function significantly improved following 16 weeks of breathing exercises in elderly subjects with asthma. A 2016 study published in the Journal of Physical Therapy Science observed that 15 minutes of breathing exercises significantly improved lung function for elderly smokers after 4 weeks. A 2014 study in the journal Integrative Medicine observed that patients with moderate to severe chronic obstructive pulmonary disease (COPD) exuded significant improvement in lung function following 12 weeks of daily breathing exercises. It appears that there is indirect evidence that WHM could likely improve lung capacity/function in the elderly with AD which could then lead to greater CSF movement, CBF, and increased brain pH levels leading to the downregulation of the AD genes.
As we touched upon above, decreased and altered neurogenesis has also been observed in AD patients. Neurogenesis is the process by which new neurons are formed in the brain. In a 2017 study published in Cell Stem Cell, the pathway for adult human neurogenesis was identified as being based upon necessitating mitochondrial electron transport and oxidative phosphorylation. A 1990 study published in the Journal of Applied Physiology found that inducing chronic hypoxia in animals induced a downregulation of oxidative phosphorylation at 55% of normal. A 2003 study in the Journal of Physiology observed that acidosis (decreased pH) inhibits oxidative phosphorylation in human skeletal muscles.
If chronic hypoxia and acidosis can downregulate oxidative phosphorylation which then negatively affects neurogenesis, is there the possibility that increased oxygen levels and pH increases can upregulate oxidative phosphorylation leading to optimized neurogenesis?
A 2018 review in the journal Frontiers in Neuroscience cites multiple animal studies indicating that exercise increases levels of brain derived neurotropic factor (BDNF) which ultimately increases neurogenesis in the hippocampus area of the brain. A 2018 study in the journal Physiological Reports provides data showing that hypocapnia (increased oxygen levels) leads to increases in vascular endothelial growth factor (VEGF). A 2002 study published in the Proceedings of the National Academy of Sciences observed that VEGF stimulates neurogenesis in vivo and in vitro. This then brings us to the endogenous DMT discussion being that exogenous forms have been observed to induce neurogenesis. Being that the EEG patterns of 20 minutes of WHM and exogenous DMT/Ayahuasca seem to have overlap based on gamma wave upregulation, there lies the potentiality that WHM upregulates endogenous DMT. There also lies the possibility that endogenous DMT/5-MEO provide neuroprotective aspects as well as anti-inflammatory responses based on in vitro studies. The concept of increased neuroplasticity from serotonergic psychedelics also adds to the conversation being that compromised neuroplasticity has been observed in Alzheimer’s disease. A 2020 write-up in the journal Frontiers in Synaptic Neuroscience outlines the proposed mechanisms (neurogenesis, neuroplasticity, reduction in neuroinflammation) with which serotonergic psychedelics could be utilized in order to address AD.
While the potential benefits of endogenous DMT upregulation to address AD are intriguing, the gamma wave increases seem equally important based on the data regarding gamma oscillation’s relationship with memory formation/retrieval. A 2019 study published in the Proceedings of the National Academy of Sciences observed that fast gamma power increases take place in the hippocampus during human episodic memory formation and that 40 Hz gamma power increases in the hippocampus during memory retrieval. Episodic memory is sensitive to the effects of age and severely impaired in Alzheimer’s disease. It’s considered to be the first memory system to decline in both normal and pathological aging. A 2007 study published in the journal Psychological Science observed that gamma oscillations distinguish true from false memory recall. According to the researchers, “Recall of a true memory is preceded by an increase in gamma oscillations in the hippocampus (bilaterally) and in the temporal and prefrontal cortices (primarily in the left hemisphere)”. A 2021 study in the journal Hippocampus found that increased coupling between theta and gamma oscillations play a key role in memory retrieval.
A 2016 study published in Nature reported that researchers exposed AD-animal models and aged animals to 5 different conditions consisting of constant light, 20 Hz flicker rate, 40 Hz flicker rate, 80 Hz flicker rate, and randomized light flicker rates for one hour. These light flicker rates caused entrainment of the brain meaning that it led to the brain’s oscillating at the same frequencies as the stimulation. The data indicated that only 40 Hz (gamma) exposure reduced amyloid beta (1-40) and (1-42) by nearly 60% compared to controls. The 20 Hz and 80 Hz frequency failed to induce any significant decrease in amyloid beta when compared to dark and light controls. A 2020 review published in the Proceedings of the National Academy of Sciences cites the various research indicating exposing AD animal models to 40 Hz light flicker and 40 Hz sound reduced the number of amyloid plaques and tau protein tangles in their brains in addition to improving the animal’s working memory, sensory processing, and spatial navigation.

It seems rather clear that normalizing or optimizing gamma oscillations could be very important in reversing continued memory degradation in AD. While much of the discussion thus far surrounding WHM and endogenous DMT pertains to inducing altered states of consciousness, I hope that I’ve outlined some of the more “grounded” aspects and potential for this method of breathing especially pertaining to AD. It seems clear that WHM can influence and reverse multiple layers of impaired physiology associated with this neurodegenerative disease. This is interesting in light of the strategies of biotechnology companies such as Alector and Athira Pharma attempting to address AD. In 2018, Alector raised $133 million to research and develop immunotherapy targets for AD while in 2020 Athira Pharma raised $85 million to test their NDX-107 drug for brain function restoration for AD.
(Excerpt from the Forbes article on Alector)
“Two of the drug candidates are focused on treating Alzheimer’s disease. One targets a triggering receptor on myeloid cells called TREM2. The other targets SIGLEC-3, a transmembrane receptor that’s expressed on cells of myeloid lineage. Mutated versions of both TREM2 and SIGLEC-3 are known to contribute to the development and progression of Alzheimer’s disease.”
The question I propose is whether merely “triggering a receptor” on myeloid cells would induce the systemic changes necessary to reverse the disease. It’s clear that if a receptor is triggered but fails to positively address the lack of CSF movement/production, sub-optimized cerebral blood flow, sub-par lung function, decreased cerebral pH, altered neurogenesis, and suppressed gamma oscillations… it wouldn’t seem very promising as a candidate to “cure” the disease. The same question would go for the drug NDX-107. It seems plausible that all layers of physiology would seemingly need to be addressed simultaneously to create a reversal of the conditions. The main issue is that it appears likely that the extracellular environment is the triggering mechanism for the downstream genetic dysregulation so without inducing a change to this extracellular environment, the signaling catalyst remains intact regardless of tinkering with receptors.
For example, a 2018 case study in the journal Medical Gas Research reports that a 58 year old woman diagnosed with rapidly progressing AD was exposed to an 8 week course of hyperbaric oxygen therapy (HBOT). HBOT involves breathing pure oxygen in a pressurized environment. The 8 week course of HBOT reversed the patient’s symptomatic decline. Prior to the treatment, positron emission tomography (PET) brain imaging revealed global and typical metabolic deficits in AD. Following the HBOT treatment, PET demonstrated a 6.5%-38% regional and global increase in brain metabolism, including increased metabolism in the typical AD diagnostic areas of the brain. The researchers outline the fact that HBOT targets numerous processes of AD including affecting the microcirculation, mitochondrial dysfunction, reducing amyloid beta, controlling oxidative stress, and reducing neuroinflammation.
A 2020 study in the journal Alzheimer’s and Dementia included 83 subjects in which included 42 AD patients, 11 amnestic mild cognitive impairment (aMCI) patients, and 30 control AD patients. The 42 AD patients and 11 (aMCI) patients were treated with 40 minutes of HBOT once per day for 20 days. The researchers then followed up with the patients one month, 3 months, and 6 months after the ending of the final HBOT session. The data indicates that a reversal of cognitive impairment took place for both AD and aMCI patients up to one month after cessation of the therapy. The benefits dissipated over time following the one month follow-up.
These results are intriguing in light of the potentiality for WHM to mimic the systemic effects of HBOT on AD when incorporating the protocol for extended periods of time on a consistent basis. These HBOT studies also preliminarily validate the systemic approach of addressing AD compared to the end-point receptor based models.
Based on the data presented thus far it would seem that utilizing any method (HBOT or WHM) that increases brain pH, CBF, CSF movement/production/drainage combined with dietary changes, optimizing sleep, 40 Hz light flicker exposure, 40 Hz sound exposure, and utilizing certain supplementation would seem rather promising as a way to properly address the AD condition.
Added Notes: It’s no secret that sleep deprivation increases various biomarkers of AD in the brain including beta amyloid. A 2019 published in Science observed that increased delta oscillations (slow wave) during sleep were specifically tied to CSF flow, drainage, and clearing of metabolic waste products during sleep. If these delta oscillations are directly tied with clearing of metabolic waste from the brain during sleep… does there lie the possibility that increasing delta oscillations during waking consciousness could provide similar benefits regarding waste clearance in the brain? Interestingly a 2011 study published in the Journal of Cerebral Blood Flow & Metabolism observed that an increase of carbon dioxide concentrations in the brain increased the power of delta oscillations. A 1999 study in the journal Undersea & Hyperbaric Medicine observed an increase in the power of delta oscillations following voluntary breath holds. A 2015 study in the journal Institute of Electrical and Electronics Engineers also observed an increase in the power of delta oscillations following breath holds. Being that WHM utilizes prolonged breath holds following deep breathing cycles, there lies the likelihood that delta oscillation power is increased during these retentions. An intriguing future study would be to utilize the same exact technique of simultaneous BOLD fMRI dynamics, EEG, and CSF measurements as in the 2019 Science study regarding sleep and CSF clearance to compare whether WHM induces similar CSF clearance during the retention phase. If this were to be the case, it would revolutionize not only AD treatment but potentially highlight the importance of optimized respiration techniques for all neurological disorders.
One thing to mention regarding utilizing WHM technique is that there are noted differences between engaging in the practice using nasal respiration versus mouth breathing. It was discovered in 1995 that the epithelial cells in the paranasal sinuses produce nitric oxide (NO). Nitric oxide is known to have potent vasodilatory properties as well as exuding antiviral properties. It would seem optimal to utilize nasal respiration when engaging in WHM. Another data point of note is the difference in CSF movement when utilizing upper chest breathing compared to abdominal breathing. A 2019 study in the journal Fluid and Barriers of the CNS observed that abdominal respiration exuded more pronounced effects on CSF movement compared to upper chest breathing. It appears as though nasal inspiration and abdominal breathing would optimize the WHM.
It’s been cited in a recent 2020 write-up in the journal Frontiers in Endocrinology that insulin resistance and impaired cerebral glucose metabolism have been consistently reported in Alzheimer’s disease (AD). A 2008 study in the journal Neurology observed that impaired insulin secretion increases the risk of AD. While the pancreas is cited as the predominant organ responsible for insulin secretion, the choroid plexus (the brain structure responsible for CSF production) also produces insulin which is modulated by serotonin. When coupling in the effects of hypoxia on decreasing insulin production, hypoxia inducing decreases in brain serotonin levels, and the depletion of serotonin in the brains of AD patients, it points back to sub-par respiratory rhythm and pH balance as one of the key underlying aspects for this condition.
While we know that cerebrospinal fluid movement is modulated by respiration, it has yet to be defined as to what drives actual CSF production. I hypothesize that inspiration not only induces CSF movement but that it also directly leads to the production of CSF. While the Na+, (K+)-ATPase and carbonic anyhydrase pathways have been implicated in playing key roles in the production of CSF, there have been no definitive studies specifically linking respiration with increased CSF production. However, studies showing the downregulation of CSF production by modulating Na+-K+ ATPase and carbonic anyhydrase via compounds or methods that alter pH could be key in better understanding the primary factors driving CSF production, not just movement. Perhaps there is a correlation between increased pH and increased CSF production and decreased pH and decreased CSF production. A 1972 study in the American Journal of Physiology observed that hypoxia reduced the production rate of CSF by 33% in animals.
Future Directions: At this point it seems clear that theoretically WHM would likely have a positive effect on AD physiology and potentially cognition. Now it’s time to test the theory with a study involving roughly 20 AD patients over the course of 12 weeks. A modest starting point would be to perform a comprehensive assessment of each subject prior to the study, have them engage in 20 minutes of WHM daily upon waking, and then redo the comprehensive assessment to verify whether any changes or benefits have occurred. It would be a very straightforward study and provide a starting point for investigating the effects of WHM on the degenerative disease known as Alzheimer’s.
E-mail me at jchavez@dmtquest.org with any comments or questions.
DMT Quest is a non-profit 501(c)3 dedicated to raising awareness and funds for endogenous DMT Research. This specific field of psychedelic research has been underfunded for many decades now. It’s time to take our understanding of human physiology, abilities, and perception to the next level. You can follow us at Facebook, Instagram, or Twitter.