Serotonin is a neurotransmitter derived from tryptophan and is primarily found in the central nervous system, blood platelets, and the gastrointestinal tract. A receptor is a protein molecule that receives chemical signals (ex: Serotonin) from outside a cell. When these chemical signals bind to a receptor, they cause some form of cellular/tissue response. Each receptor is linked to a specific cellular biochemical pathway. While numerous receptors are found in most cells, each receptor will only bind with molecules of a particular structure (ex: lock and key). Throughout the body, serotonin receptors are abbreviated as 5-HT (5-hydroxytryptamine) receptors. These 5-HT receptors are responsible for modulating the release of numerous neurotransmitters (ex: GABA, dopamine) and hormones (ex: oxycotin, cortisol). In general, serotonin is thought of as contributing to feelings of well-being.
(An alternate pathway to serotonin synthesis is proposed by Joanne Lee Colmer based on observing the effects of tryptophan depletion on patients with Tramautic Brain Injury (TBI) and Huntington’s disease (HD).)
There is much complexity within the subsets of serotonin and subsequent receptors which we will bypass in this piece. This particular discussion will revolve around the receptor known as the 5-HT2A.
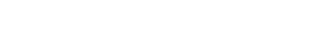
The 5-HT2A receptor is expressed near most of the serotonergic terminal rich areas. Especially high concentrations of this receptor are found in layer V of the cortex. In the periphery, it is highly expressed in platelets and many cell types of the cardiovascular system, in fibroblasts, and in neurons of the peripheral nervous system.
The significance of the 5-HT2A receptor as it pertains to DMT is in regards to it’s perceived ability to potentially mitigate (or severely alter) the visual effects of this hallucinogenic compound. A 1998 study published in Pharmacology Biochemistry and Behavior outlined the agonistic properties of DMT on the 5-HT2A receptor. This is important in the sense of being able to subjectively determine whether endogenous DMT synthesis and proposed experiences are affected by 5-HT2A antagonists (blockers).
Ketanserin is a drug that is commonly utilized to study the serotonin system, specifically the 5-HT2 receptor family. In humans it has been found to be a selective antagonist for the 5-HT2A but not 5-HT2C receptor. It also blocks the vesicular monoamine transporter known as VMAT2 (“The God Gene”).
The entire reason for this discussion is based on entertaining feedback on the piece “Measuring DMT Formation in Humans”.
One neuroscientist would present his perspective on the matter, “If ketanserin blocks a DMT trip but not a dream, then the two have different mechanisms. Start simple… just compare effects of pre-sleep ketanserin vs. pre-sleep placebo on dreams. If you alter or block dreams, you have something and might want to do further studies. My assumption is blocking a hypothetical dream molecule’s access to its key receptor will be more than just a mild alteration. 5HT2A activity is likely needed for psychedelic trip while other receptors modify/color trip.”
While this proposal doesn’t sound entirely unreasonable, there are some obvious challenges to this methodology that we will cover. This is not to mention the inherent differences between exogenously administered DMT in isolated form and the proposed mechanisms and subsequent “cascade effect” behind endogenous DMT synthesis. In Dr. Rick Strassman’s study published in 1994, he would document the effects of exogenous DMT administration on increasing blood concentrations of Beta endorphin, corticotropin, cortisol, prolactin, and growth hormone. Melatonin levels were unaffected by exogenous DMT. This would reflect a distinctly different internal physiology compared to “dream” states during sleep as melatonin concentrations peak during sleep.
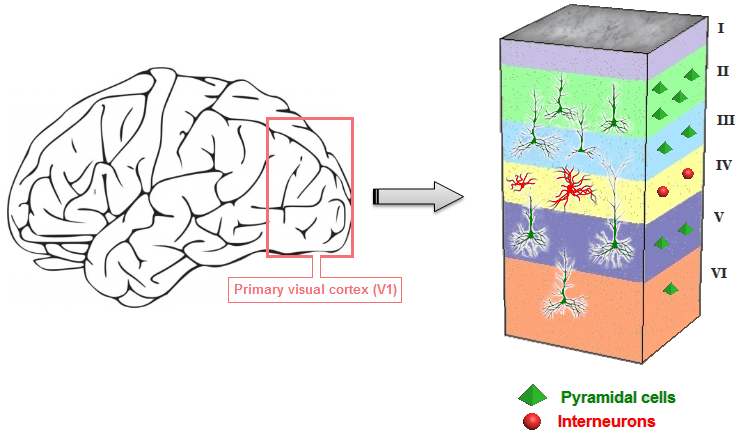
According to a 2002 study published in the American Journal of Physiology Endocrinology and Metabolism plasma melatonin levels rise an average of 500% for young adults (33 men w/average age of 23) two hours following initial sleep onset. These elevated levels remain sustained and slightly increase for 5 hours prior to declining an hour before waking. Older subjects (68 years avg.) showcased a less pronounced increase percentage wise.
(Figure 4. from the study)
Another key factor to take into account when analyzing this proposed method of subjectively measuring endogenous DMT is the fact that in Dr. Strassman’s trial, he would administer 4 different doses of DMT to the majority of the volunteers in the trial. Two doses were considered sub-hallucinogenic (0.05mg/kg, 0.1mg/kg) while 3 doses were considered to reach the hallucinatory threshold (0.2mg/kg, 0.4mg/kg). A 0.6mg/kg dose was administered to two patients who were unable to recall much of the experience and was subsequently deemed as “too much” for the official study. The importance of this is to keep in mind that elevated endogenous DMT formation might not always correlate with full blown visual effects that the general public has adopted as being synonymous with DMT itself.
There are levels…
In a 1989 study published in the journal Neuroscience Letters, it was observed the melatonin counteracted the effects of both 5-HT2 antagonists as well as agonists. This would pose a key issues in terms of utilizing Ketanserin as a subjective measure of DMT production during “dream” states as melatonin saturation in the brain is robust during these moments. It would seem logical that the effects of Ketanserin on dreams would be markedly different if administered prior to normal sleep hours (10am) compared to 3am as peak melatonin and Ketanserin levels would vary drastically. A 1999 study in Physiology & Behavior, would observe melatonin’s effect on corticosterone suggesting that melatonin has possible implications as a 5-HT2A antagonist within itself (albeit a weak one).
Psilocybin is the hallucinogenic compound found in “magic mushrooms” and is primarily responsible for the intense visual effects of this fungus. While psilocybin activates multiple serotonin (5-HT) receptors, it’s been observed that the visual perceptual alterations and hallucinations can be blocked by pretreating human subjects with 5-HT2A antagonist (blocker) Ketanserin. This has been observed in numerous studies included in Neuroreport (1998), Journal of Cognitive Neuroscience (2005), Psychopharmacology (2007), Neuropsychopharmacology (2012), and the Journal of Neuroscience (2013).
A more difficult setting to quantify includes animal studies in which Ketanserin was administered alongside the hallucinogen Lysergic acid diethylamide (LSD). Based on behavioral parameters attributed to LSD in animals, it appeared that Ketanserin blocked some of the effects of this hallucinogen as observed in the following studies: European Journal of Pharmacology (1984), Behavioural Brain Research (1985), Pharmacology Biochemistry & Behavior (2012), Neuroscience Letters (2013), Biochemical and Biophysical Research Communications (2014), and Behavioural Brain Research (2014).
As cited in a prior piece at DMT Quest, in the video clip below Dr. Steven Barker cites the unpublished dissertation by Dr. Robert Harrison of the University of Alabama at Birmingham. In this clip, Dr. Barker describes an experiment in which LSD was administered to rats which subsequently increased their endogenous levels of 5-MEO-DMT by 1000% and DMT by 400%. He states “this suggests that there is an endogenous hallucinogen neuronal system and that many hallucinogens may not actually be true hallucinogens but endogenous hallucinogen neuronal system agonists that stimulate the release of these endogenous hallucinogens which then carry out their function on perception.”
If only it were that simple…
In2016, a study published in the journal European Neuropsychopharmacology would outline the results of administering Ketanserin alongside the shamanic brew known as “Ayahuasca”. A medium dose of Ayahuasca was administered alongside 40mg of Ketanserin to 12 healthy human volunteers. The Hallucinogenic Rating Scale (HRS) developed by Dr. Rick Strassman and colleagues were subdivided into 6 sub-scales.
- Somaesthesia – effects of or relating to the body
- Affect – emotional/mood responses
- Perception – measuring visual, auditory, taste, and smell experiences
- Cognition – describing modification in thought process or content
- Volition – the capacity to interact with his/her “self” and/or environment
- Intensity – strength of the overall experience
The results were as follows in terms of the Ketanserin + Ayahuasca combination (compared to Ayahuasca alone): a 62% reduction in Affect, 56% reduction in Perception, and a 36% reduction in Intensity. There was a slight reduction but no statistically significant effect on Somaesthesia and Cognition. A deviant effect was a 76% increase in Volition (increased incapacitation).
This is an intriguing finding as it pertains to some marked differences between the effects of Ketanserin alongside LSD/Psilocybin and Ketanserin alongside Ayahuasca (DMT+MAOI). While the doses of Ketanserin were the same in 2 trials (40mg + Psilocybin) vs. (40mg + Ayahuasca), the degree of visual hallucinatory suppression appears markedly different. This presents a challenging set of issues when subjectively testing for endogenous DMT synthesis utilizing the simplistic Ketanserin protocol.
1.The effects of monoamine oxidase inhibitors (MAOIs) in regards to the DMT experience as well as Ketanserin binding sites regarding both exogenous (Harmine, Harmaline) and endogenous (6-MeO-THBC (Pinoline) & Trubulin). A 1990 study in the Journal of Neural Transmission would observe changes in the number of Ketanserin binding sites from Tribulin derivative Isatin (an MAOI). A 2000 study in the journal Antioxidant and Redox Signaling would observe a 16.9% decrease in ketanserin binding to 5-HT2A receptors in the frontal cortex of mice from Gingko Biloba (which contains MAOI Kaempferol). Being that the body produces 6 known MAO-A inhibitors (Pinoline, Tribulin A, Harman, Tryptoline, Neurocatin, & Isoquinolium derivatives) as well as 3 MAO-B inhibitors (Phosphatidylserine, Quinolic Acid, Tribulin B) their fluctuations and subsequent effects on Ketanserin binding site changes must be accounted for.
2. The subjective nature of dream interpretation and recall. While EEG analysis can give us information as it pertains to what we believe a person is experiencing while asleep, it is ultimately their ability to communicate that experience that quantifies what is actually taking place from a “dream” perspective. There are many people across the world who have very little dream recollection every night but it doesn’t necessarily disqualify endogenous DMT from being produced within those subjects. In many cases, exogenous DMT experiencers have difficulties recalling their “trips”. I refer back to the 0.6mg/kg DMT dose that was deemed “too much”.
3. The multiple receptor factor as it pertains to DMT as it’s been measured to have greater affinity for the following 14 receptors in comparison to the 5-HT2A receptor: 5-HT7, 5-HT1D, 5-HT2B, Alpha-2B, Alpha-2C, D1, 5-HT2C, 5-HT1E, 5-HT6, 5-HT5A, Imidazoline-1, Alpha-1B, Alpha-2A, & Alpha-1A. (DMT showed slightly lesser affinity for SERT, Sigma-1, 5-HT1A, receptors than 5-HT2A and has been speculated to also have affinity for Trace Amine-Associated Receptors (TAARS) and Metabotropic Glutamate receptors (mGluR2).
4. The proposed complimentary endogenous hallucinogenic compounds that coincide with DMT (N,N-dimethyltryptamine) release and their specific receptor affinity. These would include (but not limited to):5-methoxy-N,N-dimethyltryptamine (5-MEO-DMT), MAO inhibitors 6-MeO-THBC (Pinoline) & Tribulin, and 5-OH-DMT (Bufotenine). These additional compounds would obviously be projected to correlate with a significant difference in terms of physiological mechanisms that take place when comparing the proposed endogenous DMT synthesis and DMT in isolated format. It’s important to note a2015 study published in the journal Neuropharmacology that observes5-MEO-DMT as having a particular affinity for the 5-HT1A receptor which generates visual hallucinations.
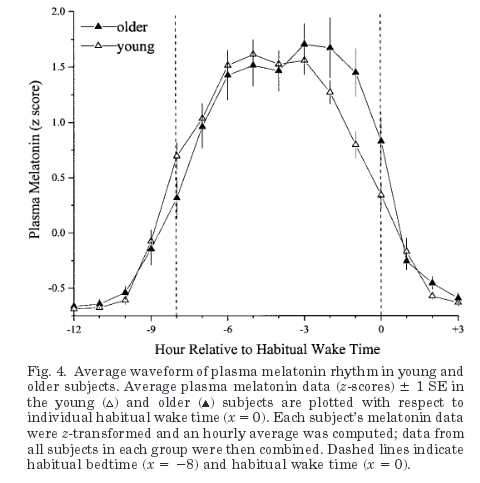
In 1990, a study was published in the journal Cardiovascular Drugs and Therapy that would consist of observing the effects of Ketanserin on the adverse effects (cold extremities, lethargy, nightmares) of beta blockade. There were 142 volunteers for the study that would take place over the course of 12 weeks. Here are some of the key notes from the study:
“Nightmares were much more common after beta blockers (16% of patients) than in our untreated patients, (8%) as previously reported. Beta blockers and serotonin antagonists reduce the duration of REM sleep. Beta blockers also disrupt sleep by increasing wakefulness and stage 1, and increase the likelihood of recalling dream episodes. Serotonin antagonists, in contrast, improve the continuity of sleep by decreasing stage 1 and prolonging deep (slow wave) sleep. Thus the addition of ketanserin to a beta blocker reduces the awareness of vivid dreams and provides improved sleep quality, as previously reported.”
“In conclusion, serotonin antagonism by ketanserin can reduce the nightmares and sleep disturbance and reverse the deterioration in peripheral circulation that may accompany treatment with beta blockers.”
In 1994, a study published in the journal Neuropharmacology would outline the effects of Ketanserin and Ritanserin on sleep. There were 8 human volunteers utilized for the study which took place over 4 nights, spaced 1 to 2 weeks apart. The results of the study in regards to Ketanserin were that it produced a dose dependent increase in slow wave sleep (SWS) duration, 17.2% for 20mg and 24.4% for 40mg. The study did not observe changes in the duration of REM sleep nor did it include subjective experiences/changes of dreams from Ketanserin administration.
In 2010, a study was published in the journal Nature of Science and Sleep that observed the effects of 5-HT2A antagonist (not Ketanserin) on people with insomnia. Much like the 1994 study, it was observed that an increase in slow wave sleep (SWS) duration takes place from numerous types of drugs that operate as 5-HT2A antagonists.
Outside of the 1990 study there are no examples of studies in which it’s been documented that Ketanserin has a marked effect on dream content or recall. A 2001 study in the journal Pharmacopsychiatry outlined the effects of 5-HT2A antagonist Trazadone on patients with PTSD with insomnia or nightmares. The results were that 72% of the patients found trazodone helpful in decreasing nightmares, from an average of 3.3 to 1.3 nights per week.
Unfortunately the decrease in nightmares from both Ketanserin and Trazadone would be difficult to quantify in terms of being attributed to the 5-HT2A receptor blockage. A 2002 study in the Journal of Clinical Psychopharmacology would observe the effects of Prazosin on patients with PTSD in terms of sleep and nightmare occurrence. The results of the study showed a marked improvement in both sleep and a reduction in nightmare occurrence. However, Prazosin is not a 5-HT2A antagonist but rather a Alpha-1 adrenergic receptor antagonist. Interestingly enough, both Ketanserin and Trazadone have Alpha-1 adrenergic receptor antagonistic properties.
It seems evident that utilizing Ketanserin (or any 5-HT2A antagonist) to analyze endogenous DMT formation during sleep in order to postulate whether humans synthesize this compound during “dream” phases is a very inexact science.
Based on the effects of Ketanserin and other 5HT2A antagonist in terms of enhancing slow wave sleep (SWS) duration, it’s not surprising that Delta & Theta wave power showed a marked increase from Ayahuasca + Ketanserin administration. It’s also not surprising to observe the significant increase in incapacitation (76%) from the combination of both substances that would coincide with increases in slow wave formation.
Since it seems evident that Ketanserin fails to fully suppress the effects of a medium Ayahuasca dose, there would be limited information derived from a Ketanserin+Sleep trial in terms of endogenous DMT. It would seem better served to develop additional studies regarding the effects of (DMT+Ketanserin), (Melatonin+DMT+ Ketanserin), (Melatonin+DMT+MAOI+Ketanserin), (Melatonin+DMT+5-MEO-DMT+MAOI+Ketanserin) in order to verify the level of suppression Ketanserin can provide regarding a DMT-based experience that might possibly mimic the cascade effect that takes place during endogenous formation. It would seem important to identify a compound (if possible) that has a distinctly pronounced effect on suppression of exogenous DMT experience in order to better quantify endogenous synthesis.
As it pertains to a Ketanserin/Dream study, it might prove more useful to administer Ketanserin alongside techniques that are projected to correlate with endogenous DMT formation while awake such as meditative states, Wim Hof Method, hypnosis, & sensory deprivation. Specific subjects that are consistently prone to having visual hallucinatory experiences from these states would need to be enrolled. This would allow for a more accurate assessment of 5-HT2A antagonist effects on endogenously produced hallucinations as the subjects can provide real-time feedback. If there is distinct alteration in terms of the subject’s regular experiences compared to pre-treatment with Ketanserin, there would be some insight offered. Dream recollection and the subsequent disturbances would seem much more arbitrary of a measurement incomparison. Perhaps if a Ketanserin/Sleep study were to be carried out, it would take place via IV administration in which the patient would be automatically injected at 3am-4am when their dream vividness and length would be optimized. Another variable to consider would be to enroll “lucid dreamers” in the study in order to verify whether there were any significant changes in terms of “lucidity”.
While not a formal study, in David Jay Brown’s recent book “Dreaming Wide Awake”, he notes that psychedelics appear to induce an increase in the lucidity of dreams in the days and weeks following initial ingestion. There is the likelihood that there is some correlation with enhanced dream lucidity following psychedelic experiences and neurogenesis in the brain observed from psychedelic compounds. Intriguingly enough, many practitioners of the “Wim Hof Method” (WHM) report increased dream lucidity after engaging in the practice for a period of time. WHM has also largely been speculated to induce endogenous DMT synthesis based on the hallucinatory phenomena experienced from the discipline as well as crossover comparison from practitioners who have experienced both WHM & exogenous DMT.
In a “sideways” related subject, selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed antidepressant drugs. The effects of SSRI’s depend on their ability to block serotonin reuptake after weeks of usage. Interesting anecdotal reports associated with SSRIs are the drastically subdued visual effects of LSD, Psilocybin, & DMT due to long-term SSRI usage. This has been implied as being directly correlated with the decrease in serotonergic receptor binding. A 2013 study in the journal Biological Psychiatry would outline the downregulation of 5-HT1A receptor binding by SSRI treatment. Staying within the same vein of discussion, if SSRI’s have a marked effect on suppressing the mentioned hallucinogenic compounds due to suppressed serotonergic receptor binding, are there any effects on dreams?
A 2001 study in the journal Sleep Research outlined the effects of SSRI’s on sleep quality and dreams of 14 volunteers (4 males, 10 females). The study would take place over the course of 31 days (7 days drug free baseline, 19 days of SSRI treatment, and 5 day acute discontinuation). The results of the study were as follows (during SSRI treatment phase): dream recall frequency was decreased, the propensity to enter REM sleep was decreased, overall degradation of sleep quality, and vividness of dreams would increase during steady state administration vs. early drug treatment.
Based on crude analysis, it would seem pertinent that in order to design a quality serotonergic antagonistic based study in terms of dreams, it would be key to block both the 5-HT2A as well as the 5-HT1A receptors. Being that DMT, 5-MEO-DMT, Melatonin, and Bufotenine all have affinity for 5-HT1A (which affects visual hallucinatory experiences) it would appear important to address this.
Based on the information provided… I don’t believe it’s that simple to deduce quality information from pre-sleep Ketanserin vs. pre-sleep Placebo in terms of “dream molecule” synthesis. The number of periphery hormones, neurotransmitters, ionic variation, CSF/CBF volumetric flux, and pH alterations that take place via respiratory fluctuations during sleep are markedly different than comparing the effects of ingestion of an isolated compound. This is even more evident when looking at the distinct systemic changes in both the body and brain (electrically speaking) during sleep/naturally induced altered states. We would be forced to inherit the assumption that the brain would not adapt to specific receptor blockage and drive electrical pulses across compensatory receptors/areas in order to drive the visual experience.
We’d also have to assume that changes in physiological mechanisms would have no effect on the half-life of serotonergic antagonists. In good conscience I cannot assume that modern science fully comprehends more than a fraction of the brain’s complexities and dynamic compensatory mechanisms especially as it pertains to it’s intertwinement with the cardiovascular and respiratory systems.It’s an interesting proposal to discuss but I believe the potential results to be too subjective and overly reductionist by nature. With a few modifications it could offer some marginally valuable but still subjective data.(A 2003 study in The Journal of Neuroscience provides some insight into the gene expression patterns in the somatosensory cortex when comparing hallucinatory 5-HT2A agonists and non-hallucinatory 5-HT2A agonist. A 2013 clinical review in Sleep Medicine Reviews discusses the wide ranging effects of many different antidepressants on dreams.)
DMT Quest is a non-profit 501(c)3 dedicated to raising awareness and funds for endogenous DMT Research. This specific field of psychedelic research has been underfunded for many decades now. It’s time to take our understanding of human physiology, abilities, and perception to the next level. E-mail me at jchavez@dmtquest.org with any comments or questions. You can also follow us at Facebook, Instagram, or Twitter.